Blood type
From Wikipedia, the free encyclopedia
A blood type (also called a blood group) is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system, and some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens, that stem from one allele (or very closely linked genes), collectively form a blood group system.[1]
Blood types are inherited and represent contributions from both parents. A total of 30 human blood group systems are now recognized by the International Society of Blood Transfusion (ISBT).[2]
Many pregnant women carry a fetus with a different blood type from their own, and the mother can form antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG, a small immunoglobulin, which can cross the placenta and cause hemolysis of fetal RBCs, which in turn can lead to hemolytic disease of the newborn, an illness of low fetal blood counts which ranges from mild to severe.[3]
Contents[hide] |
[edit] Serology
If an individual is exposed to a blood group antigen that is not recognized as self, the immune system will produce antibodies that can specifically bind to that particular blood group antigen, and an immunological memory against that antigen is formed. The individual will have become sensitized to that blood group antigen. These antibodies can bind to antigens on the surface of transfused red blood cells (or other tissue cells), often leading to destruction of the cells by recruitment of other components of the immune system. When IgM antibodies bind to the transfused cells, the transfused cells can clump. It is vital that compatible blood is selected for transfusions and that compatible tissue is selected for organ transplantation. Transfusion reactions involving minor antigens or weak antibodies may lead to minor problems. However, more serious incompatibilities can lead to a more vigorous immune response with massive RBC destruction, low blood pressure, and even death.
[edit] ABO and Rh blood grouping
Anti-A and Anti-B, the common IgM antibodies to the RBC surface antigens of the ABO blood group system, are sometimes described as being "naturally occurring"; however, this is a misnomer, because these antibodies are formed in infancy by sensitization in the same way as other antibodies. The theory that explains how these antibodies are developed states that antigens similar to the A and B antigens occur in nature, including in food, plants, and bacteria. After birth an infant's gut becomes colonized with normal flora that express these A-like and B-like antigens, causing the immune system to make antibodies to those antigens that the red blood cells do not possess. People who are blood type A will have Anti-B antibodies, blood type B will have Anti-A antibodies, blood type O will have both Anti-A and Anti-B antibodies, and blood type AB will have neither. Because of these so called "naturally occurring" and expected antibodies, it is important to correctly determine a patient's blood type prior to transfusion of any blood component. These naturally occurring antibodies are of the IgM class, which have the capability of agglutinating (clumping) and damaging red blood cells within the blood vessels, possibly leading to death. It is not necessary to determine any other blood groups because almost all other red blood cell antibodies can develop only through active immunization, which can occur only through either previous blood transfusion or pregnancy. A test called the Antibody Screen is always performed on patients who may require red blood cell transfusion, and this test will detect most clinically significant red blood cell antibodies.
The RhD antigen is also important in determining a person's blood type. The terms "positive" or "negative" refer to either the presence or absence of the RhD antigen irrespective of the presence or absence of the other antigens of the Rhesus system. Anti-RhD is not usually a naturally occurring antibody as the Anti-A and Anti-B antibodies are. Cross-matching for the RhD antigen is extremely important, because the RhD antigen is immunogenic, meaning that a person who is RhD negative is very likely to make Anti-RhD when exposed to the RhD antigen (perhaps through either transfusion or pregnancy). once an individual is sensitized to RhD antigens, his or her blood will contain RhD IgG antibodies, which can bind to RhD positive RBCs and may cross the placenta. [4].
[edit] Blood group systems
A total of 30 human blood group systems are now recognized by the International Society of Blood Transfusion (ISBT).[2] A complete blood type would describe a full set of 30 substances on the surface of RBCs, and an individual's blood type is one of the many possible combinations of blood-group antigens. Across the 30 blood groups, over 600 different blood-group antigens have been found,[5] but many of these are very rare or are mainly found in certain ethnic groups.
Almost always, an individual has the same blood group for life, but very rarely an individual's blood type changes through addition or suppression of an antigen in infection, malignancy, or autoimmune disease.[6][7][8][9] An example of this rare phenomenon is the case of Demi-Lee Brennan, an Australian citizen, whose blood group changed after a liver transplant.[10][11] Another more common cause in blood-type change is a bone marrow transplant. Bone-marrow transplants are performed for many leukemias and lymphomas, among other diseases. If a person receives bone marrow from someone who is a different ABO type (eg, a type A patient receives a type O bone marrow), the patient's blood type will eventually convert to the donor's type.
Some blood types are associated with inheritance of other diseases; for example, the Kell antigen is sometimes associated with McLeod syndrome.[12] Certain blood types may affect susceptibility to infections, an example being the resistance to specific malaria species seen in individuals lacking the Duffy antigen.[13] The Duffy antigen, presumably as a result of natural selection, is less common in ethnic groups from areas with a high incidence of malaria.[14]
[edit] ABO blood group system
The ABO system is the most important blood-group system in human-blood transfusion. The associated anti-A antibodies and anti-B antibodies are usually "Immunoglobulin M", abbreviated IgM, antibodies. ABO IgM antibodies are produced in the first years of life by sensitization to environmental substances such as food, bacteria, and viruses. The "O" in ABO is often called "0" (zero/null) in other languages.[15]
| Phenotype | Genotype |
|---|---|
| A | AA or AO |
| B | BB or BO |
| AB | AB |
| O | OO |
[edit] Rhesus blood group system
The Rhesus system is the second most significant blood-group system in human-blood transfusion. The most significant Rhesus antigen is the RhD antigen because it is the most immunogenic of the five main rhesus antigens. It is common for RhD-negative individuals not to have any anti-RhD IgG or IgM antibodies, because anti-RhD antibodies are not usually produced by sensitization against environmental substances. However, RhD-negative individuals can produce IgG anti-RhD antibodies following a sensitizing event: possibly a fetomaternal transfusion of blood from a fetus in pregnancy or occasionally a blood transfusion with RhD positive RBCs.[16] Rh disease can develop in these cases.[17]
[edit] ABO and Rh distribution by country
Country  |
O+  |
A+  |
B+  |
AB+  |
O-  |
A-  |
B-  |
AB-  |
|---|---|---|---|---|---|---|---|---|
| Australia[18] | 40% | 31% | 8% | 2% | 9% | 7% | 2% | 1% |
| Austria[19] | 30% | 33% | 12% | 6% | 7% | 8% | 3% | 1% |
| Belgium[20] | 38% | 34% | 8.5% | 4.1% | 7% | 6% | 1.5% | 0.8% |
| Brazil[21] | 36% | 34% | 8% | 2.5% | 9% | 8% | 2% | 0.5% |
| Canada[22] | 39% | 36% | 7.6% | 2.5% | 7% | 6% | 1.4% | 0.5% |
| Denmark[23] | 35% | 37% | 8% | 4% | 6% | 7% | 2% | 1% |
| Estonia[24] | 30% | 31% | 20% | 6% | 4.5% | 4.5% | 3% | 1% |
| Finland[25] | 27% | 38% | 15% | 7% | 4% | 6% | 2% | 1% |
| France[26] | 36% | 37% | 9% | 3% | 6% | 7% | 1% | 1% |
| Germany[27] | 35% | 37% | 9% | 4% | 6% | 6% | 2% | 1% |
| Hong Kong SAR[28] | 40% | 26% | 27% | 7% | 0.31% | 0.19% | 0.14% | 0.05% |
| Iceland[29] | 47.6% | 26.4% | 9.3% | 1.6% | 8.4% | 4.6% | 1.7% | 0.4% |
| India[30] | 36.5% | 22.1% | 30.9% | 6.4% | 2.0% | 0.8% | 1.1% | 0.2% |
| Ireland[31] | 47% | 26% | 9% | 2% | 8% | 5% | 2% | 1% |
| Israel[32] | 32% | 34% | 17% | 7% | 3% | 4% | 2% | 1% |
| New Zealand[33] | 38% | 32% | 9% | 3% | 9% | 6% | 2% | 1% |
| Norway[34] | 34% | 42.5% | 6.8% | 3.4% | 6% | 7.5% | 1.2% | 0.6% |
| Poland[35] | 31% | 32% | 15% | 7% | 6% | 6% | 2% | 1% |
| Portugal[36] | 36.2% | 39.8% | 6.6% | 2.9% | 6.0% | 6.6% | 1.1% | 0.5% |
| Saudi Arabia[37] | 48% | 24% | 17% | 4% | 4% | 2% | 1% | 0.23% |
| Spain[38] | 36% | 34% | 8% | 2.5% | 9% | 8% | 2% | 0.5% |
| Sweden[39] | 32% | 37% | 10% | 5% | 6% | 7% | 2% | 1% |
| Netherlands[40] | 39.5% | 35% | 6.7% | 2.5% | 7.5% | 7% | 1.3% | 0.5% |
| Turkey[41] | 29.8% | 37.8% | 14.2% | 7.2% | 3.9% | 4.7% | 1.6% | 0.8% |
| United Kingdom[42] | 37% | 35% | 8% | 3% | 7% | 7% | 2% | 1% |
| United States[43] | 37.4% | 35.7% | 8.5% | 3.4% | 6.6% | 6.3% | 1.5% | 0.6% |
| . | ||||||||
| --- Mean --- | 36.5% | 33.4% | 11.9% | 4.2% | 6.1% | 5.7% | 1.7% | 0.7% |
| Std dev | 5.3% | 5.0% | 6.2% | 1.9% | 2.2% | 2.1% | 0.6% | 0.3% |
| [show]Racial & Ethnic Distribution of ABO (without Rh) Blood Types[44] (This table has more entries than the table above but does not distinguish between Rh types.) |
|---|
Blood group B has its highest frequency in Northern India and neighboring Central Asia, and its incidence diminishes both towards the west and the east, falling to single digit percentages in Spain.[45][46] It is believed to have been entirely absent from Native American and Australian Aboriginal populations prior to the arrival of Europeans in those areas.[46][47]
Blood group A is associated with high frequencies in Europe, especially in Scandinavia and Central Europe, although its highest frequencies occur in some Australian Aborigine populations and the Blackfoot Indians of Montana.[48][49]
[edit] Other blood group systems
The International Society of Blood Transfusion currently recognizes 30 blood-group systems (including the ABO and Rh systems).[2] Thus, in addition to the ABO antigens and Rhesus antigens, many other antigens are expressed on the RBC surface membrane. For example, an individual can be AB RhD positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), and so on, being positive or negative for each blood group system antigen. Many of the blood group systems were named after the patients in whom the corresponding antibodies were initially encountered.
[edit] Clinical significance
[edit] Blood transfusion
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood groups, along with the work of a blood bank to provide a transfusion service for blood and other blood products. Across the world, blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way as medicines. In the USA, blood products are tightly regulated by the U.S. Food and Drug Administration.
Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every individual recipient is given blood that is compatible and is as safe as possible. If a unit of incompatible blood is transfused between a donor and recipient, a severe acute hemolytic reaction with hemolysis (RBC destruction), renal failure and shock is likely to occur, and death is a possibility. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood.
Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. Risks can be further reduced by cross-matching blood, but this may be skipped when blood is required for an emergency. Cross-matching involves mixing a sample of the recipient's serum with a sample of the donor's red blood cells and checking if the mixture agglutinates, or forms clumps. If agglutination is not obvious by direct vision, blood bank technicians usually check for agglutination with a microscope. If agglutination occurs, that particular donor's blood cannot be transfused to that particular recipient. In a blood bank it is vital that all blood specimens are correctly identified, so labeling has been standardized using a barcode system known as ISBT 128.
The blood group may be included on identification tags or on tattoos worn by military personnel, in case they should need an emergency blood transfusion. Frontline German Waffen-SS had blood group tattoos during World War II.
Rare blood types can cause supply problems for blood banks and hospitals. For example Duffy-negative blood occurs much more frequently in people of African origin,[52] and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood for patients of African ethnicity. Similarly for RhD negative people, there is a risk associated with travelling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia, where blood services may endeavor to encourage Westerners to donate blood.[53]
[edit] Hemolytic disease of the newborn (HDN)
A pregnant woman can make IgG blood group antibodies if her fetus has a blood group antigen that she does not have. This can happen if some of the fetus' blood cells pass into the mother's blood circulation (e.g. a small fetomaternal hemorrhage at the time of childbirth or obstetric intervention), or sometimes after a therapeutic blood transfusion. This can cause Rh disease or other forms of hemolytic disease of the newborn (HDN) in the current pregnancy and/or subsequent pregnancies. If a pregnant woman is known to have anti-RhD antibodies, the RhD blood type of a fetus can be tested by analysis of fetal DNA in maternal plasma to assess the risk to the fetus of Rh disease.[54] one of the major advances of twentieth century medicine was to prevent this disease by stopping the formation of Anti-RhD antibodies by RhD negative mothers with an injectable medication called Rho(D) immune globulin.[55][56] Antibodies associated with some blood groups can cause severe HDN, others can only cause mild HDN and others are not known to cause HDN.[3]
[edit] Compatibility
[edit] Blood products
In order to provide maximum benefit from each blood donation and to extend shelf-life, blood banks fractionate some whole blood into several products. The most common of these products are packed RBCs, plasma, platelets, cryoprecipitate, and fresh frozen plasma (FFP). FFP is quick-frozen to retain the labile clotting factors V and VIII, which are usually administered to patients who have a potentially fatal clotting problem caused by a condition such as advanced liver disease, overdose of anticoagulant, or disseminated intravascular coagulation (DIC).
Units of packed red cells are made by removing as much of the plasma as possible from whole blood units.
Clotting factors synthesized by modern recombinant methods are now in routine clinical use for hemophilia, as the risks of infection transmission that occur with pooled blood products are avoided.
[edit] Red blood cell compatibility
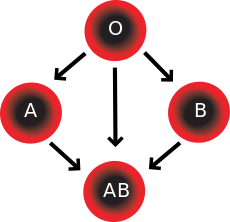
- Blood group AB individuals have both A and B antigens on the surface of their RBCs, and their blood serum does not contain any antibodies against either A or B antigen. Therefore, an individual with type AB blood can receive blood from any group (with AB being preferable), but can donate blood only to another type AB individual.
- Blood group A individuals have the A antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the B antigen. Therefore, a group A individual can receive blood only from individuals of groups A or O (with A being preferable), and can donate blood to individuals with type A or AB.
- Blood group B individuals have the B antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the A antigen. Therefore, a group B individual can receive blood only from individuals of groups B or O (with B being preferable), and can donate blood to individuals with type B or AB.
- Blood group O (or blood group zero in some countries) individuals do not have either A or B antigens on the surface of their RBCs, but their blood serum contains IgM anti-A antibodies and anti-B antibodies against the A and B blood group antigens. Therefore, a group O individual can receive blood only from a group O individual, but can donate blood to individuals of any ABO blood group (ie A, B, O or AB). If anyone needs a blood transfusion in a dire emergency, and if the time taken to process the recipient's blood would cause a detrimental delay, O Negative blood can be issued.
| Recipient[1] | Donor[1] | |||||||
|---|---|---|---|---|---|---|---|---|
| O− | O+ | A− | A+ | B− | B+ | AB− | AB+ | |
| O− | ||||||||
| O+ | ||||||||
| A− | ||||||||
| A+ | ||||||||
| B− | ||||||||
| B+ | ||||||||
| AB− | ||||||||
| AB+ | ||||||||
Table note
1. Assumes absence of atypical antibodies that would cause an incompatibility between donor and recipient blood, as is usual for blood selected by cross matching.
A RhD-negative patient who does not have any anti-RhD antibodies (never being previously sensitized to RhD-positive RBCs) can receive a transfusion of RhD-positive blood once, but this would cause sensitization to the RhD antigen, and a female patient would become at risk for hemolytic disease of the newborn. If an RhD-negative patient has developed anti-RhD antibodies, a subsequent exposure to RhD-positive blood would lead to a potentially dangerous transfusion reaction. RhD-positive blood should never be given to RhD-negative women of child bearing age or to patients with RhD antibodies, so blood banks must conserve Rhesus-negative blood for these patients. In extreme circumstances, such as for a major bleed when stocks of RhD-negative blood units are very low at the blood bank, RhD-positive blood might be given to RhD-negative females above child-bearing age or to Rh-negative males, providing that they did not have anti-RhD antibodies, to conserve RhD-negative blood stock in the blood bank. The converse is not true; RhD-positive patients do not react to RhD negative blood.
[edit] Plasma compatibility
Recipients can receive plasma of the same blood group, but otherwise the donor-recipient compatibility for blood plasma is the converse of that of RBCs: plasma extracted from type AB blood can be transfused to individuals of any blood group; individuals of blood group O can receive plasma from any blood group; and type O plasma can be used only by type O recipients.
| Recipient | Donor[1] | |||
|---|---|---|---|---|
| O | A | B | AB | |
| O | ||||
| A | ||||
| B | ||||
| AB | ||||
Table note
1. Assumes absence of strong atypical antibodies in donor plasma
Rhesus D antibodies are uncommon, so generally neither RhD negative nor RhD positive blood contain anti-RhD antibodies. If a potential donor is found to have anti-RhD antibodies or any strong atypical blood group antibody by antibody screening in the blood bank, they would not be accepted as a donor (or in some blood banks the blood would be drawn but the product would need to be appropriately labeled); therefore, donor blood plasma issued by a blood bank can be selected to be free of RhD antibodies and free of other atypical antibodies, and such donor plasma issued from a blood bank would be suitable for a recipient who may be RhD positive or RhD negative, as long as blood plasma and the recipient are ABO compatible.
[edit] Universal donors and universal recipients
With regard to transfusions of whole blood or packed red blood cells, individuals with type O negative blood are often called universal donors, and those with type AB positive blood are called universal recipients; however, these terms are only generally true with respect to possible reactions of the recipient's anti-A and anti-B antibodies to transfused red blood cells, and also possible sensitization to RhD antigens. Exceptions include individuals with hh antigen system (also known as the Bombay blood group) who can only receive blood safely from other hh donors, because they form antibodies against the H substance.[59][60]
Blood donors with particularly strong anti-A, anti-B or any atypical blood group antibody are excluded from blood donation. The possible reactions of anti-A and anti-B antibodies present in the transfused blood to the recipients RBCs need not be considered, because a relatively small volume of plasma containing antibodies is transfused.
By way of example; considering the transfusion of O RhD negative blood (universal donor blood) into a recipient of blood group A RhD positive, an immune reaction between the recipient's anti-B antibodies and the transfused RBCs is not anticipated. However, the relatively small amount of plasma in the transfused blood contains anti-A antibodies, which could react with the A antigens on the surface of the recipients RBCs, but a significant reaction is unlikely because of the dilution factors. Rhesus D sensitization is not anticipated.
Additionally, red blood cell surface antigens other than A, B and Rh D, might cause adverse reactions and sensitization, if they can bind to the corresponding antibodies to generate an immune response. Transfusions are further complicated because platelets and white blood cells (WBCs) have their own systems of surface antigens, and sensitization to platelet or WBC antigens can occur as a result of transfusion.
With regard to transfusions of plasma, this situation is reversed. Type O plasma, containing both anti-A and anti-B antibodies, can only be given to O recipients. The antibodies will attack the antigens on any other blood type. Conversely, AB plasma can be given to patients of any ABO blood group due to not containing any anti-A or anti-B antibodies.
Blood types in Japanese culture
From Wikipedia, the free encyclopedia
| Type A | |
|---|---|
| Best traits | Earnest, creative, sensible |
| Worst traits | Fastidious, overearnest |
| Type B | |
| Best traits | Wild, active, doer |
| Worst traits | Selfish, irresponsible |
| Type AB | |
| Best traits | Cool, controlled, rational |
| Worst traits | Critical, indecisive |
| Type O | |
| Best traits | Agreeable, sociable, optimistic |
| Worst traits | Vain, rude |
There is a popular belief in Japan that a person's ABO blood type or ketsueki-gata (血液型?) is predictive of their personality, temperament, and compatibility with others, similar to the Western world's astrology. This belief is also widespread in South Korea.[1]
Ultimately deriving from ideas of historical scientific racism, the popular belief originates with publications by Masahiko Nomi in the 1970s. The scientific community dismisses such beliefs as superstition or pseudoscience.[1]
Contents[hide] |
[edit] History
| This section may require cleanup to meet Wikipedia's quality standards. Please improve this section if you can. (July 2009) |
The ABO blood group system is widely credited to have been founded by the Austrian scientist Karl Landsteiner, who found three different blood types in 1900.[2] Ethnic studies did show different blood group distributions across the world (e.g. Asian people having a higher percentage of Type B). This fact was used by Nazis to further ideas of supremacy over different races.[1] Those distortions were debunked before Nazi Germany invoked race laws like the Nuremberg Laws, where the wording "German blood" is figurative for Aryan lineage.
The theory was first introduced to Japan in 1916 by Dr Kobayashi Sakae(小林栄) and Hara 来復 (原来復).[citation needed] Their mythology was made up from nonstatistical basis. He learned blood type mythology in Germany. once used as a contrary evidence to Takeji Furukawa's mythology. In 1926 Rin Hirano and Tomita Yashima published the mythology "Blood type biological related" in the medical journal of army. It was the nonstatistical and unscientific report, just as those previous ones, made up with the racism.
In 1927, Takeji Furukawa, a professor at Tokyo Women's Teacher's School, published his paper "The Study of Temperament Through Blood Type" in the scholarly journal Psychological Research. The idea quickly took off with the Japanese public despite his lack of credentials, and the militarist government of the time commissioned a study aimed at breeding the soldiers.[1] The study used no more than ten to twenty people for the investigation.
In another study, Furukawa compared the distribution of blood types among two different ethnic groups, the Formosans in Taiwan and the Ainu who live in Northeast Asia, especially Hokkaidō. His motivation for the study appears to have derived from a political incident.[3] After the Japanese occupation of Taiwan following Japan's victory over China in 1895, the inhabitants tenaciously resisted their occupiers. Insurgencies in 1930 and in 1931 killed hundreds of Japanese settlers.[3]
The purpose of Furukawa's studies was to "penetrate the essence of the racial traits of the Taiwanese, who recently revolted and behaved so cruelly". Based on the finding that 41.2% of a Taiwanese sample had type O blood, he assumed that their rebelliousness was genetically determined. The reasoning was supported by the fact that among the Ainu, whose temperament was characterized as submissive, only 23.8% had type O. In conclusion, Furukawa suggested that the Taiwanese should intermarry more with the Japanese in order to reduce the number of individuals with type O blood.[3]
The fad faded in the 1930s as its unscientific basis became evident. It was revived in the 1970s with a book by Masahiko Nomi, a lawyer and broadcaster with no medical background. Nomi's work was largely uncontrolled and anecdotal, and the methodology of his conclusions is unclear.[4] Because of this he has been heavily assailed by the Japanese psychological community, although his books are phenomenally popular.[4]
[edit] Current popularity
Discussion of blood types is widely popular in women's magazines as a way of gauging relationship compatibility with a potential or current partner. Morning television shows feature blood type horoscopes, and similar horoscopes are published daily in newspapers. In addition, a series of four books that describe people's character by blood type ranked third, fourth, fifth and ninth on a list of best selling books in Japan in 2008 compiled by Tohan Corporation.[5]
Although there is no proven correlation between blood type and personality, it remains popular with the many matchmaking services that cater to blood type. In this way, it is similar to the use of astrological signs in the west, which is also popular in Japan. Asking one's blood type is common in Japan, and people are often surprised when a non-Japanese does not know his or her own blood type.[6]
Many idols, tarento and other Japanese celebrities include a blood type statistic in their profiles, in addition to other facts such as their hobbies and star sign.
It is common among anime and manga authors to mention their character's blood types, and to give their characters corresponding blood types to match their personalities. Some video game characters also have known blood types, such as in the Street Fighter series, the Soul series, the Final Fantasy series, the Resident Evil series, the Melty Blood series, the Guilty Gear series, and the Dead or Alive series, which lists character blood types in both the manual and in-game bios. In addition, it is common for video game series, such as Gungriffon, Tekken, Animal Crossing, Metal Gear Solid 2 and Princess Maker to allow for blood type as an option in their creation modes.[citation needed]
'Crack a laugh' 카테고리의 다른 글
| The Pool Poochie (0) | 2009.09.09 |
|---|---|
| What We’re Reading . . . (0) | 2009.09.09 |
| How to Fight the Flu This Fall (No Joke!) (0) | 2009.09.06 |
| On the reappointment of Ben Bernanke (0) | 2009.09.05 |
| Unemployment hits 9.7%; stocks rally (0) | 2009.09.05 |